The FDA recently put the spotlight on the concerning side effects of marketed PI3K inhibitors for blood cancers. Similarly, investigators in the U.K. recorded a high level of side effects among head and neck cancer patients taking an experimental PI3K inhibitor by Amgen in a clinical trial.
Scientists at La Jolla Institute for Immunology (LJI) and the University of Liverpool decided to get to the bottom of the problem by studying patient samples and better understanding the effect of PI3K inhibition in mice.
In a new study published in Nature, the team provided timely clues as to why the drug class causes immune-mediated toxicities and offered a possible solution to them: dose adjustment.
The researchers focused on the PI3K-delta isoform, which is targeted by all FDA-approved PI3K inhibitors for blood cancers—Gilead Sciences’ Zydelig, Bayer’s Aliqopa, Secura Bio’s Copiktra and TG Therapeutics’ Ukoniq—as well as the subject of the new study, an Amgen candidate coded AMG319.
A phase 2 trial previously tested AMG319 as a neoadjuvant therapy for treating head and neck cancer patients before surgery. But the study was halted early after immune-related side effects forced investigators to stop treatment in 12 out of 21 patients. The most prevalent immune-related adverse reactions observed included skin rashes, diarrhea and transaminitis, which can point to problems in the liver.
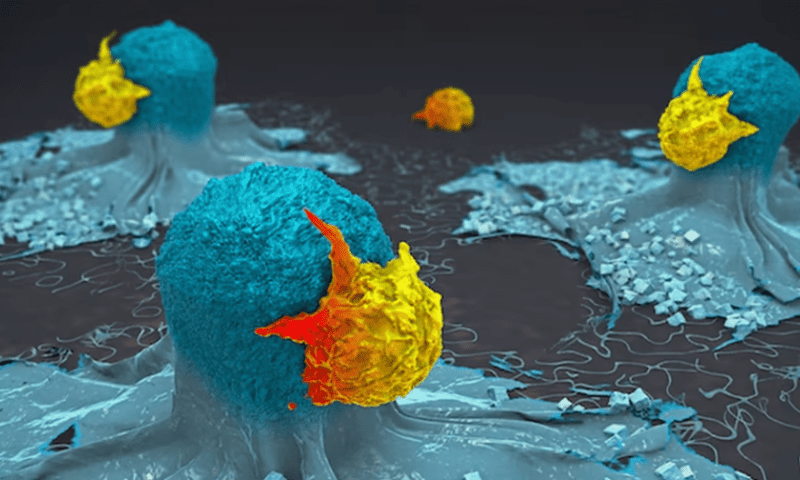
The PI3K-delta isoform is known to support the function of T regulatory (Treg) cells, which can dampen an immune response. In samples collected from the patients, the team found AMG319 treatment indeed reduced Treg cells entering the tumor and at the same time enhanced the activation and expansion of T cells, which could go after tumor cells.
In a mouse model, the researchers found similar anti-Treg effects not just in tumors but in the spleen and colon as well. Treg cells in the colon exhibited the most pronounced differences between PI3K-delta inhibitor-treated mice and animals that got placebo.
By performing single-cell genomic sequencing, the researchers found that the PI3K-delta inhibitor most notably blocked a specific subset of colonic Treg cells expressing ST2, which are critical for tissue repair and protection against chronic inflammation. These cells also expressed the immunosuppressive cytokine IL-10. The loss of the Treg cells was accompanied by the expansion of two pathogenic T-cell subtypes, which the researchers suggested caused inflammation.
The researchers hypothesized that transiently removing Treg cells might be enough to overcome the immunosuppression of tumor cells without causing too much toxicity in healthy tissues. They tested continuous dosing of PI3K-delta inhibitor, an intermittent four days on, three days off dosing regimen, and an infrequent dosing with two days on treatment followed by five days off.
Turns out, the intermittent dosing schedule significantly inhibited tumor growth in mice without inducing pathogenic T cell response in the colon.
Lack of dosing optimization was exactly the problem the FDA has criticized of existing PI3K inhibitor drug developers. For those marketed therapies, drugmakers sought the highest tolerable dose but failed to properly examine whether lower doses could achieve similarly effective anti-tumor activity with lower toxicities, the FDA said in a review document of PI3K inhibitors for an advisory committee meeting in April. At relatively high doses, those PI3K drugs appeared to shorten blood cancer patients’ life expectancy over the longer term because of the severe side effects they cause.
“More robust dose exploration trials to clarify the relationship between [tumor response] and toxicities would have potentially avoided selecting an excessively toxic dose with its resultant concerning trends in [patient survival],” FDA reviewers wrote in the document.
While the immune-mediated side effects are already observed in blood cancer patients who have received multiple prior treatments, they become more prominent and detrimental in less pretreated patients and in solid tumors. That’s likely because treatment-naïve patients have a more robust immune system to launch a harmful inflammatory response, the researchers at LJI and the University of Liverpool observed. Besides, blood cancers like chronic lymphocytic leukemia have intrinsic immunosuppressive effects.
Based on the new findings, the researchers suggest “decreased dosages or an altered” PI3K-delta inhibitor treatment regimen will be required in solid tumors to take advantage of anti-tumor benefits while limiting toxicity.
In addition, the findings could be applicable to other immunotherapies that affect Treg cells, including CTLA-4 inhibitors like Bristol Myers Squibb’s Yervoy, the team argues.
The researchers are now designing a clinical trial to test the intermittent dosing strategy in humans.