Despite CAR T-cell therapies’ high efficacy against certain blood cancers, many patients can relapse, and solid tumors simply don’t respond to existing options. That’s mainly because tumors develop various tactics that can exhaust or dumb T cells.
Now, a research team led by scientists at the University of California, San Francisco (UCSF) has uncovered that a gene called RASA2 is important to the regulation of T-cell immunity. Using CRISPR to inactivate the gene helped TCR and CAR T cells become more resilient and sensitive than control cells and prolonged survival in mice carrying either liquid or solid tumors, the team reported in a study published in Nature.
“By knocking out one individual gene, we’ve created cells that are not just potent tumor cell killers but also more persistent killers over a long period of time,” Julia Carnevale, M.D., at UCSF and the study’s first author, said in a press release.
“We’ve succeeded in engineering better, stronger, longer-lived T cells that we think will improve treatment of both blood and solid cancers,” Alex Marson, M.D., Ph.D., at UCSF and a co-leader of the study, said in the release.
Cell therapies that are engineered from a patient’s own T cells face multiple challenges in their fight against cancer. Tumors create a hostile microenvironment for T cells to survive, and repeated exposure to tumor antigens could also lead to T-cell dysfunction.
Looking for genetic clues that could boost the efficacy of engineered T cells, the UCSF-led team developed a model that mimics the multiple immunosuppressive conditions in tumors and performed large-scale CRISPR screens to turn off each gene.
The researchers identified several immune regulators that could help T cells resist those suppressive conditions. Among the hits, the scientists took a special interest in RASA2, because they had previously linked removal of the gene to enhanced T-cell function and improved cancer killing in lab dishes without the immunosuppressive environment.
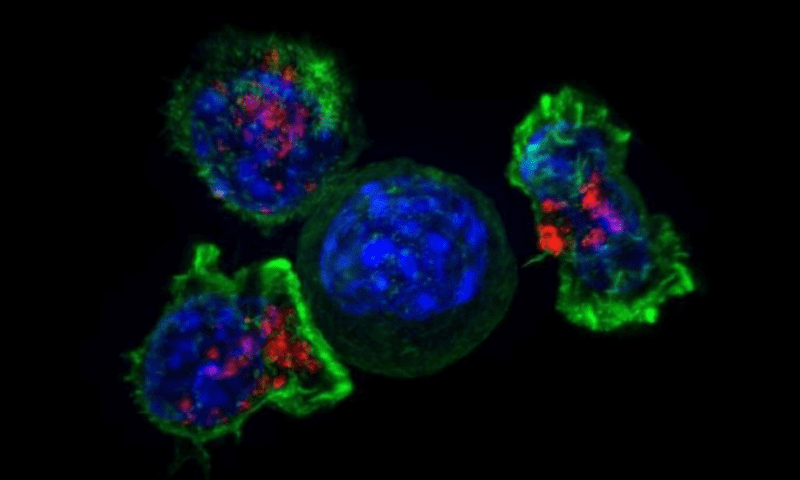
Indeed, TCR T cells with inactivated RASA2 were better at killing cancer cells in lab dishes under immunosuppressive conditions than control-edited T cells. Similarly, in an assay of chronic antigen exposure, both CAR T and TCR T cells with RASA2 ablated by CRSPR-Cas9 appeared more active and maintained effective cancer killing, whereas control-edited T cells’ ability to control cancer cell growth declined with each stimulation.
The team also engineered CD19-targeted CAR-T cells with either disrupted RASA2 or a functional gene and co-cultured them with leukemia cells expressing various levels of CD19. Some patients eventually fail CAR-T treatment because tumors can reduce target antigen expression in a phenomenon known as antigen escape so that the T cells can’t recognize them anymore.
RASA2 removal appeared to sensitize CAR-T cells to low antigen levels, the team found. In leukemia cells with low CD19 expression, CAR-T cells with inactivated RASA2 showed increased cancer killing compared to controls.
Finally, the team tested the effect of inactivating RASA2 in TCR and CAR T cells in different mouse models bearing melanoma, leukemia and bone cancer. Those RASA2-deficient engineered T cells outperformed control counterparts at reducing tumor burden and extending the lives of the rodents.
Digging into the bone marrow of a mouse model of leukemia, the researchers found significantly higher numbers of CAR-T cells and lower number of leukemia cells in mice treated with the RASA2-edited CAR-T cells than in those that got control CAR-T cells. The RASA2-ablated CAR-T cells in the bone marrow showed lower expression of exhaustion biomarkers and “clearly outcompeted” controls in terms of persistence, the team said.
What’s more, when mice were re-challenged with new leukemia cells, the novel CAR-T cells again outperformed control CAR-T cells in reducing tumor burden and increasing survival, the team found, suggesting the RASA2 ablation strategy can improve CAR-T cell persistence in living beings.
Scientists have always tried to add or delete components in CAR-T cells to enhance their anticancer ability. Also using CRISPR screens, scientists at the Curie Institute in France recently pinpointed a protein called suppressor of cytokine signaling 1 (SOCS1) as a brake on CD4+ T cell proliferation. They suggest inactivation SOCS1 opens the possibility to optimize CAR-T cell therapy.
A team at St. Jude Children’s Research Hospital recently used CRISPR screens to show that inhibiting the protein complex cBAF could direct naïve T cells to become more long-lasting memory T cells. CAR-T cells transiently treated with a cGAF inhibitor during activation showed better anti-tumor response than untreated cells.
The current UCSF-led study showed that “RASA2 ablation increases the potency and the persistence of T-cell therapies, two key domains in which these therapies have been failing clinically,” the researchers wrote in the study. With the ability to fight immunosuppressive factors, RASA2 loss represents “a promising new strategy for generating more effective T cell therapies for hematological and solid tumor indications.”