Breast cancer patients are surviving for longer than ever before, but the survival rates for those with brain metastasis remain dismally low. Once metastatic cancer cells take up root in the brain, patients can die in as little as just a few months.
Now, after seeing brain metastases retreat in a new preclinical mouse model for metastatic breast cancer, a group of scientists based at the University of Lausanne and the University of Fribourg in Switzerland is making the case for testing small-molecule focal adhesion kinase inhibitors, or FAK inhibitors, in patients. In a study published Wednesday in Science Translational Medicine, they reported on findings that suggest that gap junction proteins, or connexins, that mediate FAK activity are the key to metastatic breast cancer cells’ ability to colonize in the brain.
“Considering the limited therapeutic options for brain metastatic disease in cancer patients, we propose FAK as a therapeutic candidate to further pursue in the clinic,” the research team wrote in the paper.
FAK inhibitors have shown promise in early-stage clinical trials for patients with various types of primary solid tumors, but, while seven FAK inhibitors are in phase 1 or phase 2 trials, only one of them is looking at the use of the drugs in patients with metastatic disease. FAK mediates signaling events involved in cell survival, proliferation and migration. Around 20 years ago, it was first shown to be overexpressed in some types of solid tumors and has since been implicated in metastasis.
The scientists sought to build upon previous work that showed the involvement of connexin proteins in brain colonization by cancer cells, a key therapeutic target of late compared to older treatments that focused on the dissemination step of metastasis. First, though, they needed a better mouse model. Most models of breast cancer brain metastasis are based on cancer cells moving through the bloodstream after being injected into an artery or the heart, as opposed to spontaneously disseminating from a primary tumor site the way they do in the clinical setting.
To that end, the team injected the mammary glands of immunodeficient mice with primary breast cancer cells, which subsequently led to brain metastases in more than half of them. The researchers derived cell lines from those tumors and then injected them into immunocompetent mice, where they again formed brain metastases. From these, they developed a cell line that led to brain metastasis in 100% of the mice when injected into the breast tissue, giving them a model that more closely resembled the metastatic pathway in humans.
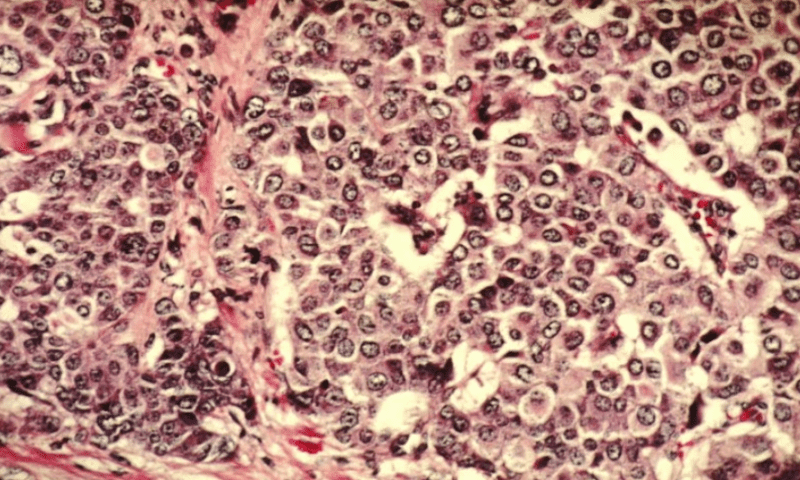
Next, the researchers set out to elucidate connexins’ involvement. They conducted transcriptome analysis of brain metastatic and non-metastatic tumor cells in mice as well as in human cells from three breast cancer types. In both cases, they found that a gene encoding for a connexin protein—Cx31 in mice and Cx43 in humans—was significantly upregulated.
Cx43 significance was validated by the fact that Cx43 was expressed to a similar degree as the brain metastases in each of the three tumor types. In addition, silencing the Cx31 gene in the metastatic cells and transplanting them in mice resulted in fewer brain metastases, indicating that the connexin protein they had identified was indeed playing a role, and later experiments confirmed that connexin was involved specifically at the point of colonization.
The scientists then sought to figure out how exactly Cx31 was moderating colonization. Knowing that FAK had been found to regulate cell adhesion and survival during breast cancer progression, they came up with a hypothesis: Cx31 and its human homolog would activate FAK in brain metastatic cells. A series of cell culture and immunofluorescence studies showed that FAK was upregulated in human brain metastatic cells compared to those from primary tumors and had been activated by Cx31.
Further research showed that Cx31-mediated FAK activation controlled the activity of another important player in brain tumor metastasis, nuclear factor-kappa beta (NF-ĸB), and that activation of NF-ĸB via FAK resulted in expression of proteins involved in cellular matrix adhesion—promoting metastatic tumor cell colonization and survival.
With a mechanism mapped out, the scientists then turned their attention to FAK inhibitors. Using molecules developed by Pfizer and Verastem Oncology, they implanted mice with the brain metastatic breast cancer cells they had developed previously. After 14 days, they treated the mice by mouth with one of the two drugs. Both prevented metastasis formation.
Finally, the scientists implanted human tumor cells lines in mice. Using imaging to track the tumors’ progress, they treated the mice just as lesions formed in the brain, modeling clinical conditions. The FAK inhibitors prevented the lesions from growing further.
“Together, these in vivo preclinical observations point to FAK targeting as an attractive strategy to further exploit for the management of brain metastases in breast cancer,” the researchers concluded.
Editor’s Note: This article has been updated to include an additional FAK inhibitor that is under investigation for treating metastatic pancreatic cancer.