New research that helps explain why KRAS mutations drive pancreatic cancer suggests that monotherapy isn’t sufficient to eliminate it but that combining KRAS inhibitors with immunotherapy might be the key.
On Aug. 24, The University of Texas MD Anderson Cancer Center published a pair of studies in Developmental Cell and Cancer Cell that describe experiments showing how KRAS inhibitors—a hot class of drug development with agents from Roche, Amgen and Mirati and others currently in clinical trials—by themselves weren’t enough to completely kill off tumor cells. The Cancer Cell study also showed that combining Mirati’s KRAS G12D inhibitor MRTX1133 with immune checkpoint inhibitors led to improved tumor regression, clearance and increased survival in mice compared to using the drugs alone.
“These studies show that KRAS inhibition works, but monotherapy delivers only a transient response, especially when dealing with late-stage tumors,” co-corresponding author and MD Anderson researcher Anirban Maitra said in a press release. “Leveraging the immune system by combining KRAS inhibitors with immunotherapy was able to bring about the full effects of these drugs and provide the best possible survival benefits in our models.”
While two KRAS inhibitors have already been approved as monotherapies, researchers and companies are looking at combinations to avoid resistance and improve efficacy. There’s evidence that some pairs already work in animals: For instance, a team at the University of California San Diego School of Medicine recently found that Mirati’s FDA-approved KRAS inhibitor adagrasib, or Krazati, and Boehringer Ingelheim’s ERBB gene inhibitor afatinib, or Gilotrif, improved survival rates and was more effective at clearing tumors than either drug alone.
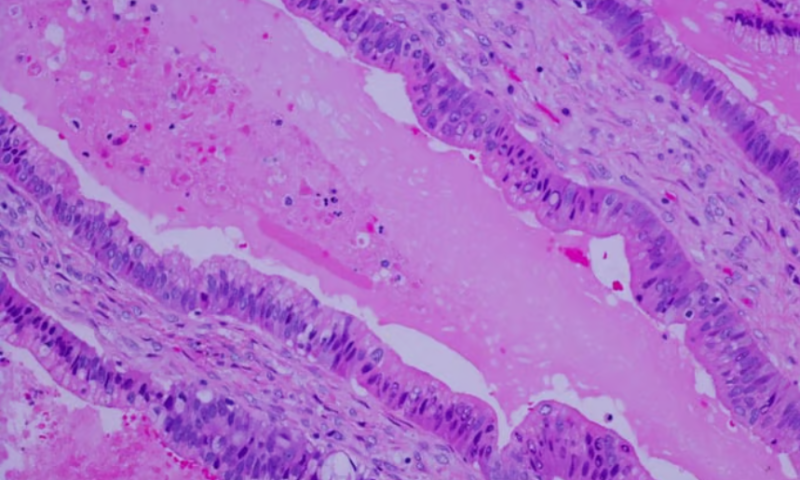
The new studies further supported a combo approach, first by showing how KRAS mutations keep cancer cells alive. In the Developmental Cell paper, the MD Anderson team used mouse models with a variety of genetic changes known to be linked to KRAS mutations to look at the functional role of the KRAS gene. They found that, in those models, suppressing the gene activated what’s known as the Fas pathway, a series of interactions between a group of proteins within cells that leads to their death. The takeaway: The KRAS gene helps tumors survive by blocking expression of the Fas pathway, so they don’t undergo normal cell death.
But while inhibiting KRAS did unblock expression of the Fas pathway in KRAS-mutated mouse models with cancer and reduce their tumors, it wasn’t enough to keep them from eventually growing back. To that end, in the study published in Developmental Cell, the researchers combined MRTX1133 with various immune checkpoint inhibitors that activate CD8+ T cells—a type of immune cell suppressed by the tumor microenvironment and a common target of cancer immunotherapies—in 16 different lab models with early- and late-stage pancreatic tumors. This approach increased the number of cancer cells cleared, kept the tumors at bay for longer and improved survival in the mice.
Researchers from Mirati and MD Anderson are evaluating MRTX1133 in humans in a phase 1 clinical trial, enrollment in which is ongoing. The new findings will support further clinical applications for the drug, the MD Anderson team said in the press release.