Since the first patient received allogeneic hematopoietic cell transplantation (allo-HCT) to treat thalassemia, an inherited blood disorder affecting hemoglobin, in 1982, the therapy has rapidly grown in popularity. More than 8,000 transplants took place in 2021 according to the National Marrow Donor Program, and the procedure is now used to treat various blood cancers, inherited diseases, and sickle cell disease.
Allo-HCT comes with the risk that the foreign, curative donor cells will attack the recipient’s cells, causing acute graft-versus-host disease (aGvHD). A paper published in Nature on July 10 shows that an enzyme from a bacteriophage extended the lives of mice afflicted by aGvHD, suggesting that the protein could have potential as a treatment for allo-HCT patients suffering from it as well.
Allo-HCT is an intensive procedure. The patient must first have their own immune system weakened by chemotherapy or another conditioning treatment before stem cells from a donor’s blood are infused into the patient’s bloodstream. Conflict between donor and recipient cells is common, with about 30% to 60% of patients developing aGvHD following the transplant. Symptoms can range from a mild rash and diarrhea to liver damage and can be life-threatening.
A large 2020 study, led by Marcel van den Brink, M.D., Ph.D., found that disruption of the gut microbiome is linked to aGvHD, with lower microbial diversity in the gut of allo-HCT patients associated with a greater risk of death. This disruption is often caused by the flourishing of Enterococcus bacteria, which exclude helpful bacteria from the microbial community and also reduce levels of secondary bile acids, which normally help suppress the immune system and prevent GvHD.
“We kept on finding that it was Enterococcus that had the greatest likelihood to lead to dominance in those first weeks after allogeneic transplant,” van den Brink, president of City of Hope Los Angeles and National Medical Center, told Fierce Biotech. “There’s really something specific and almost universal about that,” added van den Brink, who was not involved with the new study, but did peer review it before it was published.
This known link between the microbiome and aGvHD inspired Kosuke Fujimoto, M.D., Ph.D., a medical researcher at Osaka Metropolitan University and the University of Tokyo in Japan, and colleagues to screen the bacteria in the guts of allo-HCT patients.
The researchers analyzed fecal samples from 46 transplant patients, more than half of whom were acute leukemia patients. DNA sequencing showed that 30 of the patients had gut microbiomes dominated by Enterococcus bacteria, including Enterococcus faecalis, a species known to influence aGvHD severity. E. faecalis can be killed by antibiotics, but the researchers found that the microbes form gooey masses called biofilms, which protect individual cells from antibiotics.
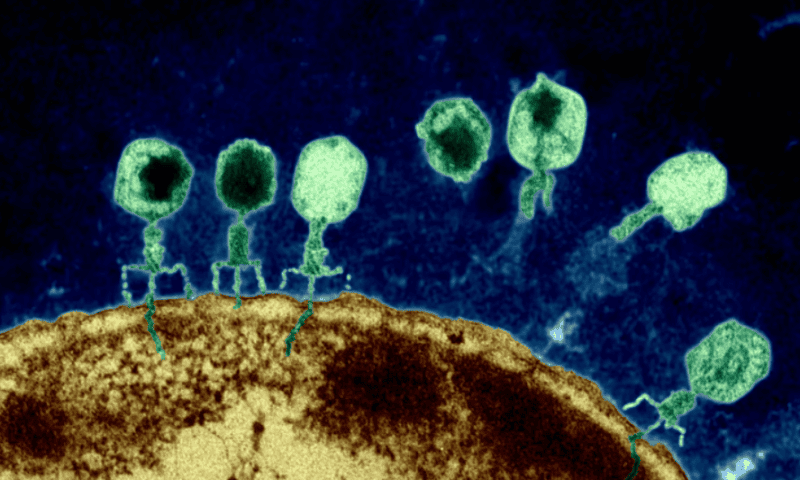
Because the team previously found that bacteriophages—viruses that prey on bacteria—produce proteins called endolysins that can kill another type of bacteria, Clostridioides difficile, they decided to see if phage that infect E. faecalis are wielding a similar weapon.
Scouring through DNA from E. faecalis revealed nine viral endolysins, one of which the team isolated. Pitting the endolysin against E. faecalis biofilms sourced from the patients proved incredibly effective, as the enzyme broke down the protective goo while showing no harmful effects toward beneficial bacteria.
To show that this endolysin’s anti-biofilm activity could be useful in aGvHD, the team next implanted E. faecalis from patients into the guts of mice and then induced aGvHD in them by injecting them with bone marrow cells and splenic T cells. Treating these mice with 200 micrograms of oral endolysin three times a week for three weeks resulted in lower levels of E. faecalis in their feces compared to controls, as well as lower levels of interferon gamma, which is involved in inflammation.
Treated mice also survived longer; almost all the treated mice were still alive 25 days after the transplant, whereas about half of the untreated mice survived that long.
“Our discovery of the endolysin enzyme holds promise for future applications in preventing or treating acute GvHD,” Fujimoto said in a press release. According to the release, endolysins could lead to a new class of drugs targeting bacterial biofilms, which are also implicated in a wide range of other diseases, from urinary tract infections to atherosclerosis.
“I believe endolysin has a great potential as a therapeutic agent in GvHD control,” Xue-Zhong Yu, M.D., an immunologist at the Medical College of Wisconsin who was not involved in the study, said via email. “Due to its specificity, endolysin is expected to have little or no toxicity” to patients, he added.
Van den Brink agreed on the endolysin’s promise. “It’s one of these papers where you both have something that is really clinically relevant, but a beautiful, mechanistic story also,” he said. “They have developed a strategy that really has some chance to be translated into the clinic.”