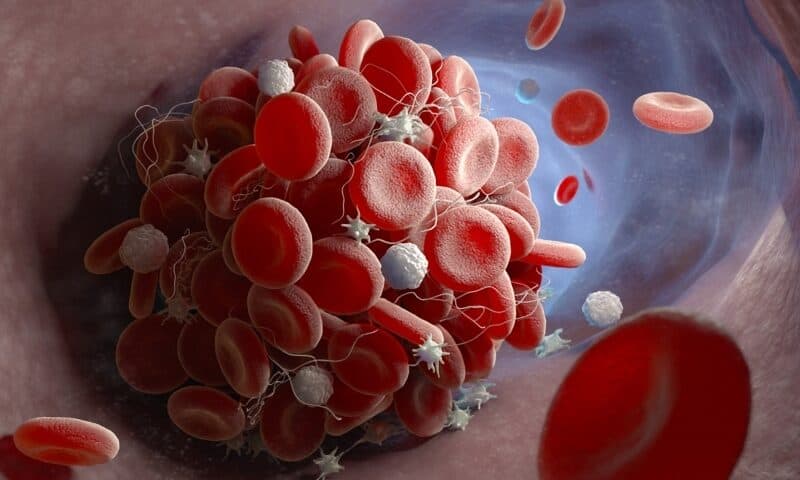
Existing clot busters have one major drawback: They prevent heart attack by indiscriminately blocking platelet function, thereby increasing the risk of uncontrolled bleeding.
Now, a research team led by Monash University in Australia has found a way to target platelet activation in a manner that appears to specifically address the pathological clumping of blood without tampering with normal processes that prevent uncontrolled bleeding.
In a new study published in Science Translational Medicine, the scientists showed that inhibiting a protein called PI3KC2a could alter how platelets react to a change in blood flow, which can promote the formation of clots, a common cause of heart attack or stroke.
The Monash-led team started by searching for tiny changes within platelets that occur during the pathological setting of a heart attack. PI3KC2a expression in platelets drew their attention. Mice that were genetically edited to lack PI3KC2a were completely protected against arterial thrombosis without any impact on bleeding, the team found.
The PI3K-AKT-mTOR pathway is a well-known therapeutic target for cancer treatment. But what exactly is the role of PI3KC2a, a class II PI3K, in platelets?
The researchers used electron microscopy to cut ultra-thin “slices” of the platelets from the mice. They found that the platelets’ internal membranes changed in a way that prevented the platelets from clumping with each other or sticking to blood vessel walls when there was a change in blood flow.
“It is this blood flow perturbation which is a hallmark and predictor of a heart attack,” Justin Hamilton, the study’s senior author, explained in a statement. “This enzyme allows the platelets to respond to this blood flow change and to ‘gear up’ their capacity to clot, causing an attack.”
The researchers went on to develop inhibitors of PI3KC2a, and to further examine a lead candidate, dubbed MIPS-21335. In human blood samples, the drug had anti-thrombotic effects, they found. Then they compared the effects with those of two commonly used anti-platelets, aspirin and a P2Y12 receptor inhibitor. The scientists discovered that MIPS-21335 was still effective when the force of flowing blood on the surface of the blood vessels increased, while the two gold-standard treatments became impaired under that stress.
In mice, MIPS-21335 prevented thrombosis but had no impact on bleeding time or blood loss. In contrast, aspirin significantly prolonged bleeding time and increased blood loss, the team reported.
A team led by the University of Oxford recently is also focusing on addressing blood-flow stress as a strategy to prevent heart diseases. The Oxford researchers found that a type of the Plexin D1 protein on the endothelial cells that line artery walls could be leveraged to rein in the potentially harmful response to blood-flow changes.
Scientists at the Wyss Institute at Harvard University are tackling the excessive bleeding problem with anti-platelet drugs another way. They recently created “decoy” platelets that were unable to bind to the blood vessel wall and that prevented normal platelets from clumping. The anti-clumping activity could be reversed by transfusing functional platelets, they suggested.
The next step for the the Monash team is to refine MIPS-21335 for potential clinical trials in people facing a high risk of cardiovascular disease, Hamilton said.