Inflammatory bowel disease, or IBD, is tough to treat, and existing therapies don’t work for everyone. Now, researchers have discovered a previously unknown link between a “master regulator” of gut processes and inflammatory molecules involved in IBD—and have a drug that could treat it.
“We revealed something that wasn’t known, and through that discovery can make a prediction in an area that desperately needs a new kind of fundamental approach to the disease mechanism,” Ron Evans, Ph.D., head of the Gene Expression Laboratory at the Salk Institute who led the research team behind the findings, told Fierce Biotech Research. “We have the molecule that is a model for a drug we could actually use in humans.”
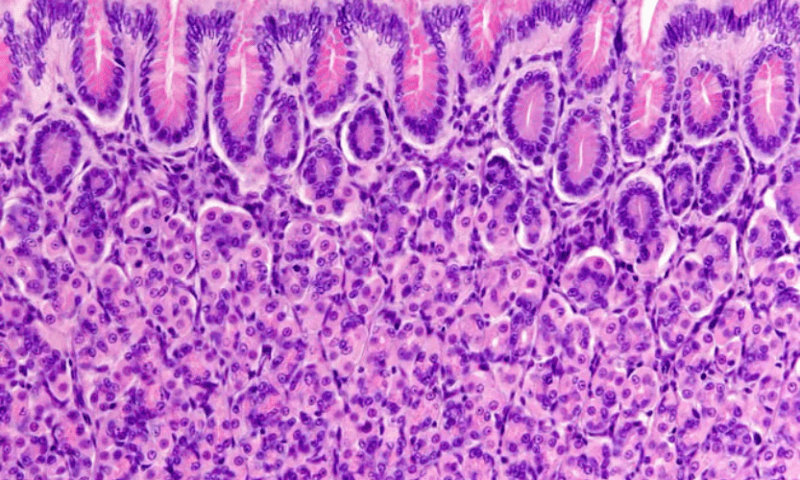
In a study published Dec. 12 in Proceedings of the National Academy of Sciences, Evans’ team described how they discovered that the farnesoid X receptor, or FXR, is found both on intestinal cells and on a set of inflammatory molecules that drive IBD. When the scientists gave mice with IBD a drug called FexD that stimulates the FXR receptor, it both reversed and protected them from the inflammation-driven changes to the gut lining that characterize the disease.
“[FexD] has a really beneficial effect on reducing inflammation induced by ILCs [innate lymphoid cells],” Evans said. “It’s a breakthrough in the sense that until now there’s really been very little we’re able to do with those cells from a therapeutic point of view.”
FXR is a steroid receptor found in the epithelial cells that line the intestines. It’s activated in response to bile acids, compounds that are synthesized in the liver and secreted into the intestines to absorb lipids from food. When FXR detects bile acids, it readies the digestive system for food by switching on and off the genes for cell processes involved in fat metabolism, blood sugar regulation and digestion. This controls the inflammation in the gut that’s inherent to eating.
Evans’ lab discovered FXR in 1995 and has been working to understand its many functions ever since. After learning its role in metabolism, they developed a drug called fexaramine that made headlines for its ability to control weight gain and blood sugar levels in mice by stimulating FXR expression, essentially mimicking bile acids. FexD is an updated version of that drug and has been shown to prevent changes in cancer-linked changes in gut stem cells. Unlike other drugs, FexD was formulated so that it doesn’t move into the bloodstream and affect other systems.
“We engineered it with the property of only acting in the gut, so it doesn’t get absorbed in the body—just the intestine,” Evans said. “You take it, it does its job in the intestine and you poop it out.”
But while FexD remains in the gut, it turns out that its effects aren’t limited to the epithelial cells there. After finding that gut inflammation turned off FXR, the scientists checked to see whether FexD could turn it back on again. Initially, they thought the drug was working on the intestinal cells alone.
“But when we ran these models of [Crohn’s disease, another inflammatory bowel condition] or inflammatory bowel disease, we realized that we were seeing something independent from the gut,” Evans recalled. “We thought, well, could it be working on Crohn’s or inflammatory bowel disease directly?” That turned out to be correct. When they analyzed the immune cells involved in IBD, the researchers found that FXR was present on ILCs. An overabundance of ILCs in the gut has previously been implicated in inflammatory bowel disease.
When the scientists gave FexD to mice with IBD, they found that the drug bound to FXR on both the intestinal cells and the ILCs. This led to changes in gene networks that ultimately reduced the number of ILCs in the intestines to levels found in healthy mice. It also reinstated processes that had been disrupted by inflammation.
“[FexD] hacks into the genetic circuit and turns back on a network that was turned off,” Evans explained. “FXR is the switch, and we know how to flip it back on with the drug.”
The fact that FXR is present on both the ILCs and the intestinal cells is a testament to the synchronicity of evolution, Evans added. It’s likely that the two types of cells evolved to have complimentary roles.
“Nothing in science makes sense in the absence of evolution,” Evans said. “This is a multimillion-year process, every trick has been tried.”
While the lab’s focus isn’t IBD per se—Evans is primarily interested in genomic networks—the team was happy to have found another potential use case for FexD. They plan to continue studying the gene networks in ILCs that change when the drug is administered, working with immunologists who will parse individual members of the ILC family to see how it affects them.
“I’m interested to see how we can take our expertise and actually activate the gene networks that we know are the heart and soul of what those cells do,” Evans said. By figuring out exactly what FexD is doing and how, they hope to build a drug that will treat IBD in humans.