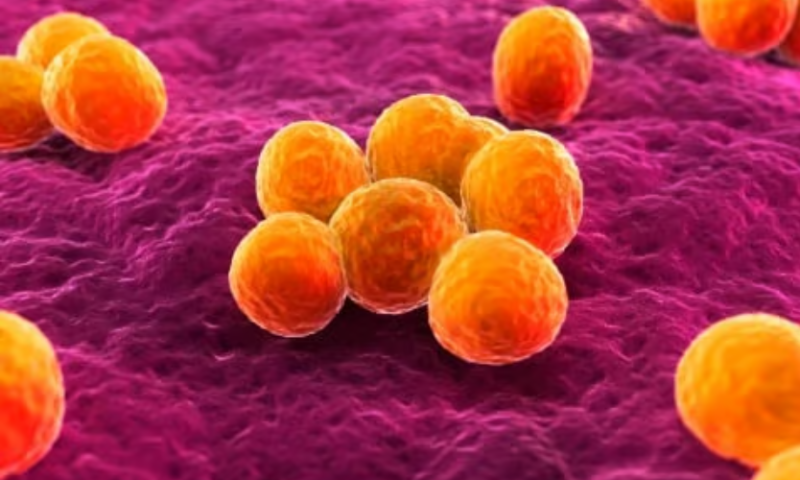
A team of researchers led by Integrated Biosciences and the Massachusetts Institute of Technology have used a new form of artificial intelligence to discover a class of antibiotics capable of killing methicillin-resistant Staphylococcus aureus, or MRSA.
In an article published Dec. 20 in Nature, the team described how they identified the compounds using an “explainable” AI model—that is, one where it’s clear how the model came to its conclusions. The drugs were effective against MRSA in mice both when applied topically and systemically.
“This paper announces the first AI-driven discovery of a new class of small molecule antibiotics capable of addressing antibiotic resistance, and one of the few to have been discovered overall in the past 60 years,” Felix Wong, Ph.D., cofounder of Integrated Biosciences and first author on the new Nature paper, told Fierce Biotech Research in an email. He added that the company’s work “promises to accelerate antibiotic drug discovery by making deep learning models more explainable and providing publicly available large datasets and models that accurately predict selective antibiotic activity.”
Antibiotic resistance has concerned researchers for decades, but the problem has gained more attention in the past few years as the drugs’ widespread use in medicine and agriculture have pushed bacteria to evolve better defenses against them. Scientists have recently turned to AI for help.
In February 2020, the MIT lab of James Collins, Ph.D.—who is a founding member of Integrated Biosciences’ scientific advisory board and helped lead the new study—used machine learning to reveal that the old diabetes drug halicin had broad antibiotic properties.
But as powerful as AI may be for finding new drug candidates, researchers typically don’t know exactly how the models make decisions. One of the team’s goals with the new study was to open up the black box to explain how the conclusions were reached.
“In drug discovery, black box models have been prevalent because they are powerful and accurate, if not able to be interpreted or understood,” Wong said. “However, we think that next-generation approaches to drug discovery, like the one developed in our Nature paper, will start to make use of ‘explainable’ models, which are models that also tell you why they are producing specific outputs.”
For their new study, the researchers chose to focus on finding new antibiotics for MRSA on account of its resistance to first-line medications and its propensity for dangerous blood infections. They started by screening a set of 39,000 antibiotics, natural products and other molecules for their ability to stop MRSA from growing. This data was then used with a program called Chemprop to train neural networks to classify whether or not a compound was likely to inhibit MRSA based on its chemical structure, supplementing the models with additional data to improve accuracy. They built similar neural networks that could predict whether the compound would be toxic to human cells.
Next, they engineered their trained models to explain “not only which compounds have selective antibiotic activity, but also why—in terms of their chemical structure,” Wong said. To do so, they used Monte Carlo tree searchers, the same type of algorithm that underlies Google DeepMind’s gaming program AlphaGo.
“Our explainable approach provides a blueprint for how the infinitude of druglike small molecules (~1060 compounds) can be efficiently mined for new antibiotics using deep learning,” Wong said.
The researchers used their models to comb through more than 12 million compounds and parse out what fit the neural networks’ rationales—in other words, had chemical structure that was predictive of anti-MRSA activity.
“This is a powerful approach because we can go beyond using deep learning to identify single compounds to test, and instead use deep learning to identify entire classes of compounds,” Wong said. “The rationales provide specific chemical insights as to what the models look for.”
The models ultimately led the researchers to a set of 283 compounds, most of which fell into one of five different structural groups. One of the groups provided two compounds that analyses showed were likely to have characteristics that would make them good candidates for drug development, such as high oral bioavailability. They work by dissipating the pH on the bacterial membrane, for which they are selective—and, thus, non-toxic to human cells.
“This mechanism of action is noteworthy because we show that bacteria does not readily evolve resistance to the compounds,” Wong said. “This is likely because lipid membranes are harder to modify than proteins.”
They proceeded to test one of them topically in mice with MRSA infections limited to their thighs and systemically in mice with thigh infections that had spread to the bloodstream.
The compound reduced MRSA load ten-fold in both models. In the systemic model, signs of illness were reduced even in mice with severe disease who were on their way to developing sepsis.
Given those results, the team plans to continue developing the compounds for the clinic. They’ll collaborate with nonprofit Phare Bio, of which Collins is a cofounder, to do so. Integrated Biosciences will also continue building out explainable AI models for drug discovery, focusing on aging and age-related pathways.
“We are very excited about the possibilities our Nature paper opens up,” Wong said.