Generating insulin-producing pancreatic beta cells from stem cells to replace those that have been destroyed by the immune system is a promising approach to treating diabetes. But it has proven challenging to make the cells responsive to glucose changes and to prevent an immune attack after the cells are transplanted.
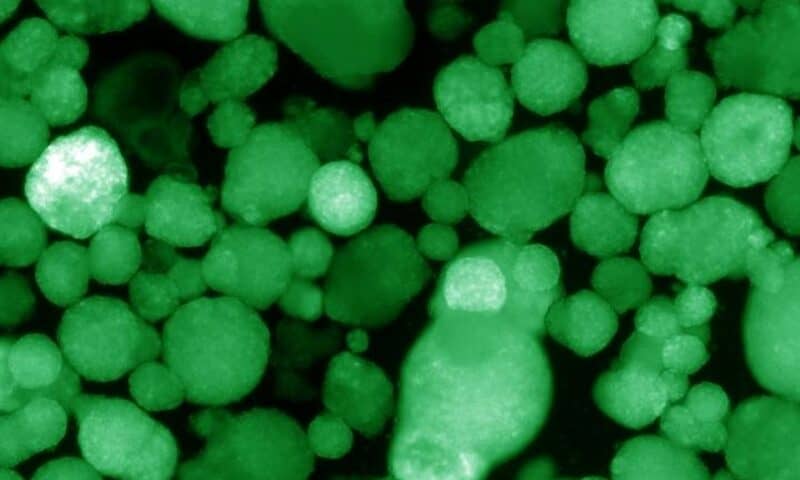
Now, scientists at the Salk Institute have found a potential solution to those problems. They created functional, 3D cell clusters—called human islet-like organoids (HILOs)—that restored glucose control in mouse models of diabetes without triggering immune rejection, they reported in Nature.
The team successfully protected HILOs from the immune system without genetic manipulation. If the method succeeds as a therapy, patients who receive islet transplants could potentially avoid the need for chronic immunosuppression, which can increase the risk of dangerous infections, the team suggested.
Researchers at Salk previously discovered that increasing the expression of a receptor called ERR-gamma could give beta-like cells derived from human-induced pluripotent stem cells (iPSCs) enough energy to mature into functional cells that responded to glucose changes by producing insulin.
In the new study, the researchers found that a protein called WNT4 was able to turn on the ERR-gamma-driven maturation of the beta cells. By exploiting that pathway, they built mature cells in a 3D environment that mimics the human pancreas, creating HILOs.
To tackle the complex problem of immune rejection—including autoimmune responses—the team took a page from a popular cancer immunotherapy.
Subsets of cells in healthy islets were found to express PD-L1, a known checkpoint that keeps immune reactions in check. To investigate whether PD-L1 expression would protect HILOs from immune rejection, the team generated two types of HILOs.
The Salk researchers developed a method to induce PD-L1 in HILOs using repeated short exposures to the protein interferon gamma. When transplanted into diabetic mice with healthy immune systems, those HILOs reduced glucose levels for more than 40 days, whereas the efficacy of cells lacking interferon gamma treatment decreased, the team reported.
Scientists have long been looking for ways to overcome the obstacle of immune rejection in the transplantation of islets to treat diabetes. A team from Georgia Tech, the University of Louisville and the University of Michigan devised a hydrogel with the protein Fas ligand, which they showed could “educate” immune cells to accept foreign islets.
The lack of high-quality islet donors has also prompted efforts to use stem cells to generate beta cells. Sigilon Therapeutics has an ongoing collaboration with diabetes giant Eli Lilly that’s focused on developing encapsulated beta-cell therapy based on iPSCs. The Massachusetts biotech recently raised $80 million in series B financing.
Moving forward, the Salk researchers plan to test the HILOs transplants in mice for longer periods of time to confirm their effects and safety before starting a clinical trial. “This is the first study to show that you can protect HILOs from the immune system without genetic manipulation,” Michael Downes, a co-author of the study, said in a statement. “If we are able to develop this as a therapy, patients will not need to take immune-suppressing drugs.”