In 2022, on the alpine shores of Lake Maggiore in northern Italy, longtime friends Samuel Bakhoum, M.D., Ph.D., and Stefano Santaguida, Ph.D., were catching up. Pandemic restrictions had prevented the two from seeing each other for years, but, at a small conference in the lakeside town of Stresa, they seized the opportunity to share what they’d been working on recently—the collapse of micronuclei in cancer cells.
“We were so happy and excited to be together in real life,” Santaguida, a molecular biologist at the European Institute of Oncology and the University of Milan, told Fierce Biotech in an interview. “We were working on two separate aspects at the very beginning, without knowing of each other’s work.”
Teaming up to tackle the problem has now resulted in two papers published Aug. 29 in the journal Science. The studies explain in mechanistic detail how micronuclei rupture and collapse in cancer cells, an important process that drives cancer progression. By getting tangled with mitochondria, micronuclei are exposed to reactive oxygen species that alter the behavior of a key repair protein and over-activate a protein-destroying pathway.
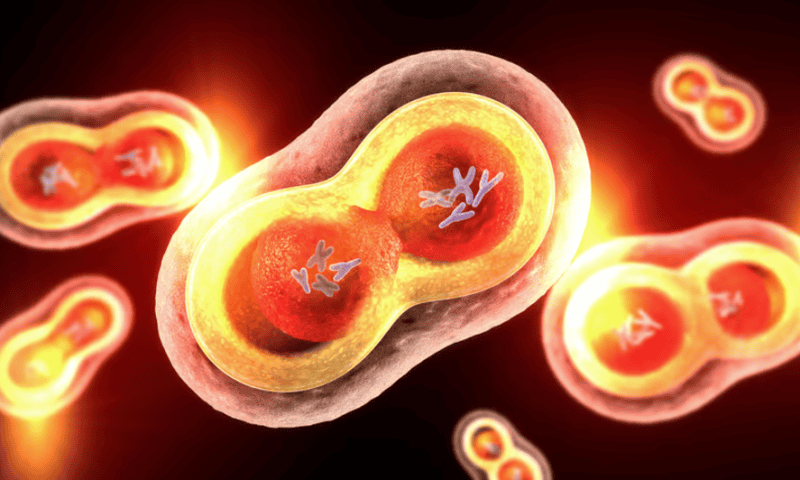
A hallmark of cancer cells is aneuploidy, when a cell has too few or too many chromosomes. This happens during cell division, when chromosomes can get left behind and not incorporated into the nucleus of a new daughter cell. A stranded chromosome forms a shoddy nuclear membrane around itself, which is much smaller and less functional than the main nuclear envelope that surrounds the nucleus. These micronuclei can then break apart, leaving the chromosome exposed to the cellular elements.
“That rupture process underlies a lot of the means by which micronuclei seem to drive cancer progression,” Bakhoum, a cell biologist at Memorial Sloan Kettering Cancer Center in New York City, told Fierce in an interview.
Enzymes in the cytoplasm break chunks off the free-floating DNA, leading to mutations that can spur new cancer traits or alter how genes are expressed. And the cell can also confuse the loose chromosome for a virus, sparking inflammation that can lead the tumor to evolve immune resistance.
Melody Di Bona, Ph.D., a cancer biologist working in Bakhoum’s group, was observing cervical cancer cells under the microscope when she noticed that micronuclei tended to get tangled up with mitochondria. “My hypothesis when I started to look at cells was that mitochondria were actually entering the micronucleus,” Di Bona told Fierce in a joint interview with Santaguida.
Investigating further, she instead found that the chance of rupture greatly increased as the micronucleus was exposed to more and more toxic forms of oxygen-containing molecules leaking from the mitochondria, called reactive oxygen species (ROS). Through a series of experiments, she pieced together how the membrane unraveling unfolds.
Tumors tend to be low on oxygen, which the mitochondria normally need to function; when oxygen is low, nitric oxide binds in its place instead, which produces ROS as a byproduct. ROS are unstable and can steal electrons from other molecules, messing with their forms and functions. Di Bona found that ROS take electrons away from amino acids called cysteines in the protein CHMP7, changing its form so that it abnormally binds to another protein called LEMD2 that sits inside the micronuclear membrane. What’s more, ROS damage also prevents CHMP7 from being kicked out of the cell.
“LEMD2 is already in the membrane,” Bakhoum said. “And now imagine a protein that’s aggregating inside, right underneath, and pulling it away.” The force of CHMP7 tugging at LEMD2 causes the micronucleus’s membrane to collapse and rupture.
Di Bona first looked at CHMP7 because it’s normally a key part of a nuclear membrane repair enzyme called ESCRT-III. But this enzyme is prevented from patching up the rupturing micronucleus due to the actions of another protein called p62.
“p62 is a protein that has its own life,” Santaguida said. “It works in the cells by recognizing proteins or organelles that have to be degraded,” targeting them for a process called autophagy.
Santaguida’s team found that ROS from mitochondria also alter p62, ramping up its activity to send proteins down the autophagy pathway. This overreactive p62 degrades the repair enzyme ESCRT-III, further dooming the micronuclear membrane to collapse. To connect p62 with cancer prognosis, the team analyzed data from the tumors of 875 gastric cancer patients and found that higher levels of p62 were correlated with shortened survival.
“The higher the levels of p62, the higher the likelihood to get a worse prognosis,” Santaguida said. “It’s a prognostic marker that can be employed in the clinic tomorrow.”
In addition to the prognostic power of p62, the collapse mechanism presents several other potential targets for new drugs. Therapies could target cysteines in CHMP7 and push them away from a pathological path, Bakhoum said. And numerous other molecules play bit parts in the process too, like kinases in the nuclear factor κB pathway—targeting them could reduce the odds of micronuclei rupturing and causing cancer progression.
Chromosomes in cancer cells are starting to attract more attention from biotechs. Bakhoum is a co-founder and scientific adviser of Volastra Therapeutics—a biotech focused on chromosomal instability—and also serves on the scientific advisory board of precision oncology company Meliora Therapeutics.
“We can’t suppress chromosome instability [in cancer] because the cat’s out of the bag, but can we at least kneecap it?” Bakhoum said. “Can we intervene in a way that prevents all the bad consequences and sequela of micronuclear rupture?”