Bowel cancer has been making headlines for its mysterious rise among young people. Now, researchers have identified a potential new target for treating it.
In a study published Jan. 26 in Science Advances, scientists from Australian National University (ANU) reported that a protein called Ku70 appears to stop cells with cancer-causing DNA damage from turning cancerous. Given the protein’s function and involvement in anti-cancer pathways, it might make an ideal target for treating bowel cancer, the researchers said.
“Our research shows that Ku70 can ‘cool off’ cancer cells and mop up damaged DNA,” lead author Abhimanu Pandey, Ph.D., a postdoc at ANU, said in a press release. “The protein prevents the cancer cells from becoming more aggressive and spreading throughout the body, essentially deactivating them and keeping them in a dormant state.”
Previous research has linked the absence of Ku70 to colon cancer in mice and to what’s known as chromosomal instability in human colorectal cancer, a sign of poor prognosis. The terms “colon cancer” and “bowel cancer” are often used interchangeably, but colon cancer is most accurately described as a subtype of bowel cancer. Ku70 expression, or lack thereof, has been associated with breast cancer risk, cervical cancer survival and lymphoma, too.
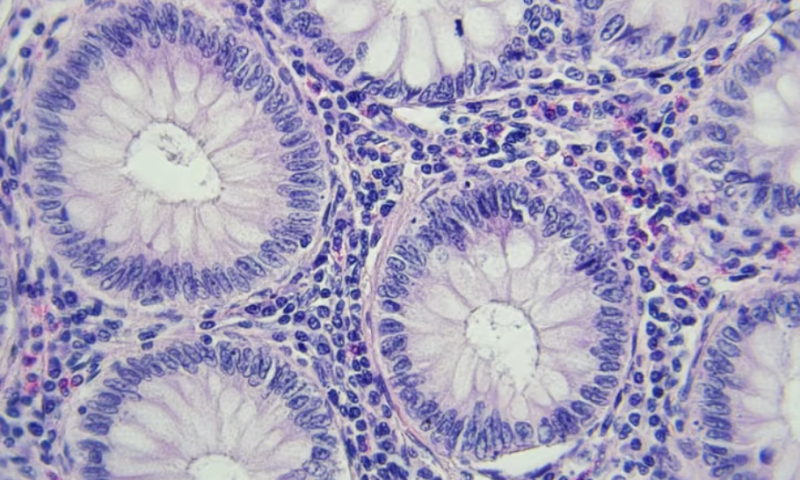
The goal of the new study was to determine Ku70’s role in tumor progression in the context of bowel cancer. First, the researchers showed that colon cancer mouse models with a gene mutation that leads to lower-than-normal levels of Ku70 had more tumors and more severe disease than wildtype animals. They were also more susceptible to developing colitis, or inflammation of the large intestine, despite having the same gut flora as mice without the mutation.
A second set of experiments backed up those findings. Mice with two different genetic mutations—the one that leads to lower levels of Ku70 plus one that causes them to spontaneously form polyps in their intestinal tract, similar to a gene that causes hereditary colon cancer in humans—developed more tumors in the small intestine and colon than mice with the gene mutation for spontaneous polyp formation but normal levels of Ku70 did. Together, the findings indicate that “[insufficiency of] Ku70 increases the susceptibility to intestinal cancer,” the researchers wrote in their paper.
Additional cell experiments revealed a likely explanation. When Ku70 detects DNA damage, it forms a complex called a signalosome with two other proteins, Ras and Raf, that activates anti-tumor and anti-colitis pathways. But there are caveats to this: Mutations in the pathways that the Ku70-Ras-Raf signalosome activates could lead to abnormal cell growth, and the trigger for the complex formation may affect whether its downstream effects hinder or drive cancer proliferation.
Dysregulation of the same anti-tumor pathway turned on by the Ku70-Ras-Raf signalosome—the Ras-ERK pathway—has been implicated in other types of cancer development, the researchers noted, including colorectal tumors. But attempts to target it in some bowel cancer types have ended in resistance, even though they’ve worked against melanoma and other cancers.
“Although targeting Ras-ERK has been successful in the treatment of several human cancers including melanoma, more innovative and effective therapeutic approaches are warranted to target the Ras-ERK signaling pathway in colorectal cancer,” the scientists wrote.
A more effective approach might be to target Ku70 directly, the researchers said in their paper. Small molecules that interact with the part of the Ku70 protein that recognizes DNA damage and its binding to other molecules might allow researchers to manipulate it “with more precision” without disrupting the protein’s other functions, such as DNA repair, they wrote. Furthermore, future research that illuminates how Ku70 interacts with Raf and Ras could be helpful not only for finding new bowel cancer treatments but other types of cancer involving pathways that are activated by the signalosome.
“While these findings could aid in the design of therapies benefiting patients with intestinal cancer who have a reduced expression of Ku70, our findings could also provide insights into the treatment of cancers with hyperactivated Ras-ERK signaling,” the researchers wrote.
Meanwhile, the findings also suggest that the presence or lack of Ku70 in precancerous polyps could predict how well a patient is likely to respond to treatment, co-author Si Ming Man, Ph.D., pointed out in the ANU press release.
“Our research shows Ku70 is a good immune biomarker,” Man said. “We know early detection and treatment is vital to overcoming not only bowel cancer but potentially other cancers as well.”