Most cancer immunotherapies primarily rely on T cells to neutralize tumors. But in two new studies, scientists at Dana-Farber Cancer Institute and Stanford University have described novel immuno-oncology approaches, showing that leveraging other components of the immune system may achieve better antitumor effects.
In a Nature study, a team led by Dana-Farber developed a cancer vaccine that targeted both T cells and natural killer (NK) cells in a two-pronged attack to prevent tumor cells from evading an immune attack.
In another study published in Science Immunology, a Stanford team found that adding Dynavax’s vaccine adjuvant to Dragonfly Therapeutics’ interleukin-12 (IL-12) drug and injecting it directly into the tumor could mobilize B cells and induce a systemic antitumor response thanks to close collaboration between B cells and T cells.
Both teams suggest their methods represent promising cancer therapies to enhance an antitumor response or prevent patients from relapsing.
Cancer vaccines work by eliciting a T-cell response directed at specific antigens on tumor cells’ surface. But tumor cells can develop various mechanisms to interfere with antigen presentation to T cells, thereby hiding themselves from being recognized by the immune system. What’s more, each individual’s tumor antigens may be different, making it difficult to devise a cancer vaccine that can treat many patients.
For their vaccine, the Dana-Farber scientists, led by Kai Wucherpfennig, M.D., Ph.D., targeted two surface proteins: MICA and MICB. The proteins may increase their expression under stress conditions such as DNA damage. They then bind to and activate T cells and NK cells to clear out the troubled cells. But tumor cells can escape from this immune response by slicing MICA and MICB and shedding them.
The new vaccine-induced antibodies inhibited MICA/B shedding by tumor cells to undetectable levels and recruited a diverse population of T cells and NK cells to tumors in mice.
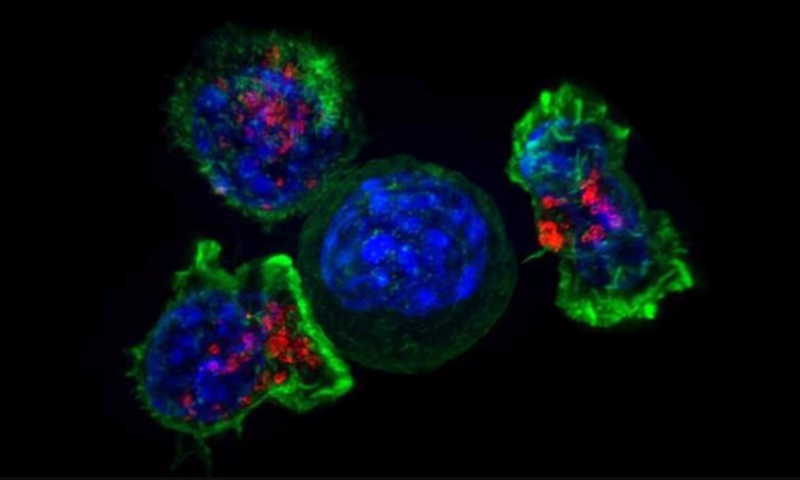
In a mouse model of aggressive melanoma, an MICB vaccine significantly shrank—and in some cases eradicated—tumors, while control mice suffered from major tumor growth. The team also tested the vaccine in mice with melanoma that’s resistant to current immunotherapies. Again, 50% to 75% of mice remained tumor-free beyond day 100 after treatment with the vaccine. Further analyses showed that both T cells and NK cells were required for effective control of the tumors.
Based on the positive efficacy in mice and some immunogenicity and safety results in monkeys, the Dana-Farber scientists said they’re now planning a first-in-human study for the vaccine. The vaccine “may also be of interest in combination with local radiation therapy, because DNA damage enhances MICA/B expression by cancer cells,” the researchers wrote in the Nature study.
For their study, the Stanford team, led by Ronald Levy, M.D., found that B cells unexpectedly contributed to the shrinking of distant tumors after treatment with a local immunotherapy.
The cytokine IL-12, by activating immune cells, is known as a potent antitumor agent. But systemic toxicity is a major hindrance for its adoption as a treatment. The Stanford team tried injecting a low-dose regimen of Dragonfly Therapeutics’ modified IL-12 drug administered locally to a tumor to reduce toxicity while taking advantage of its therapeutic potential. Through a deal signed in 2020, Bristol Myers Squibb has licensed Dragonfly’s IL-12 candidate, coded DF6002 or BMS-9896415, for cancer treatment.
The Stanford scientists further added Dynavax’s vaccine adjuvant CpG SD-101 as a stimulus to achieve a more potent T-cell immune response. Across multiple mouse models of lymphoma, colon cancer, triple-negative breast cancer and melanoma, the combination therapy led to local and distant tumor control and significantly increased survival of the animals.
While the treatment was meant to enhance a T cell-mediated response, the scientists surprisingly found that B cells were also essential in this systemic response. Clearing out B cells with an anti-CD20 antibody before and during the combo treatment eliminated the full-body effect, the team found.
After further investigation into the B cells’ behavior, the team found the B cells gave rise to tumor-specific antibodies. And in lymph nodes near the first tumors, they presented tumor antigens to T cells. Those experienced T cells then traveled to distant tumors and killed them off.
“Our data suggest that, in the future, the role of B cells should be investigated in other forms of tumor immunotherapy,” the Stanford team wrote in the study, “and that agents providing B-cell stimulation […] might be added to T cell stimulating approaches to enhance the potency and specificity of immunotherapeutic regimens.”