Researchers at Roche have developed a novel antibiotic with the ability to fight a dangerous drug-resistant bacteria that kills in up to 60% of infections.
In a pair of articles published Jan. 3 in Nature, Roche and Harvard University scientists described how they developed a new antibiotic that is effective against carbapenem-resistant acinetobacter baumannii—also known as CRAB—in mice. The drug, zosurabalpin, works by interrupting construction of the bacteria’s outer membrane.
“The ongoing research into zosurabalpin, as well as a second novel class of antibiotics being developed by Roche in human clinical studies, will help uncover new biology about the construction of bacterial membranes,” Michael Lobritz, M.D., Ph.D., global head of infectious diseases at Roche Pharma Research & Early Development, said in a statement provided to Nature. “Our goal is to contribute new innovations to overcome antimicrobial resistance, one of the biggest infectious disease challenges to public health.”
CRAB is a common culprit in hospital-acquired sepsis and other infections, and is at the top of the list of both the World Health Organization’s and the Centers for Disease Control’s “priority pathogens” for which new drugs are urgently needed. As its name implies, CRAB is resistant to all antibiotics including the last-resort drug carbapenem. While infections have declined in recent years thanks to preventative measures, according to the CDC’s 2019 report on antibiotic resistance, the bacteria killed 700 people in 2017 and added about $281 million in healthcare costs.
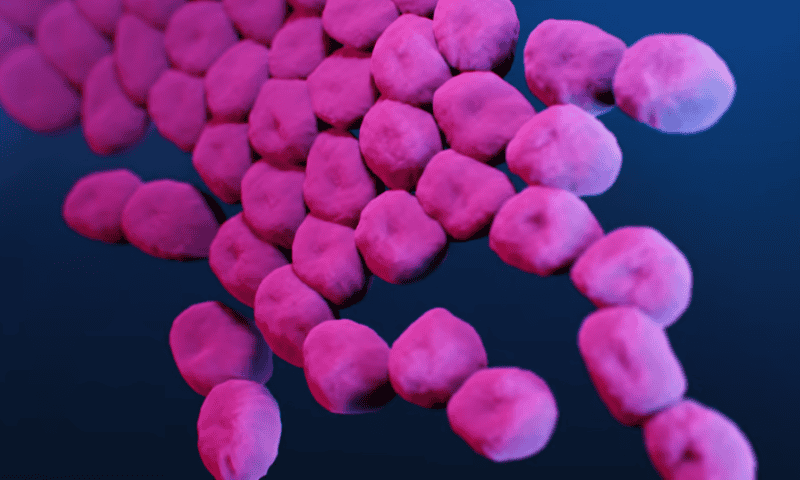
Like many other multi-drug resistant bacteria, such as some strains of Pseudomonas aeruginosa and E. coli, CRAB is gram-negative. Unlike gram-positive bacteria, gram-negative bacteria are encased in an outer cell membrane made up of molecules called lipopolysaccharides. These protect the bacteria from its surrounding environment and can evolve to make it more resistant to threats, including antibiotics.
To see if they could develop a new drug that could overcome CRAB’s resistance, the researchers turned to a class of molecules called tethered macrocyclic peptides. Earlier studies on the compounds had revealed little antibiotic activity, but a screening of more than 45,000 of them showed that one was able to selectively kill A. baumannii. After a little tweaking, they tested the resulting drug, zosurabalpin, in mouse models of CRAB infection in pneumonia, a thigh wound and sepsis. The drug was effective in reducing the bacteria in all three groups and improved the rate of survival in the sepsis models. It was also effective in killing A. baumannii in more than 100 clinical samples.
Looking more closely at its mechanism of action, the researchers found that the drug works by inhibiting a bacterial protein complex called LptB2FGC. This blocks the lipopolysaccharides from being transported to the surface of the bacterium, where they would normally form its outer membrane. Instead, the lipopolysaccharides build up to toxic levels inside the microbe, ultimately killing it.
While the researchers didn’t see any signs that the bacteria were developing spontaneous resistance to zosurabalpin, they did identify some mutations in the genes that encode LptB2FGC that could make it much less effective. This presents a unique challenge because A. baumannii doesn’t always need lipopolysaccharides “to be viable,” as researchers Morgan Gugger and Paul Hergenrother, Ph.D., wrote in a commentary that accompanied the Nature papers.
“The bacterium can halt [lipopolysaccharide] synthesis if necessary for survival—potentially rendering zosurabalpin ineffective against [those microbes],” they wrote. However, this would also make the bacteria less harmful, they added. On top of that, because zosurabalpin is highly specific for A. baumannii, it’s unlikely to damage “good” gut microbes—a problem with broad-spectrum antibiotics, Gugger and Hergenrother wrote.
Roche has already completed two phase 1 clinical trials on the drug involving 64 male and female participants. The only side effects were infusion-related reactions—things like fever, blood pressure changes, nausea and headaches related to the immune response—in nine subjects.
“Given that zosurabalpin is already being tested in clinical trials, the future looks promising, with the possibility of a new antibiotic class finally on the horizon for invasive CRAB infections,” Gugger and Hergenrother wrote.