A protein-degrading drug might offer a new treatment for Alzheimer’s disease, according to the results of a study published March 1 in ACS Central Science.
In the article, researchers from South Korea’s Kyung Hee University College of Pharmacy, in collaboration with biotech Prazer Therapeutics, laid out how they used a small molecule that conducts targeted protein degradation, or TPD, to break up a hard-to-tackle form of the enzyme p38 MAPK. The drug both improved cognition and reduced amyloid beta plaque buildup in the brains of Alzheimer’s mouse models.
The biotech world has been hot for TPD drugs for the past several years, especially for cancer. While there are different classes, they generally work by exploiting the intercellular ubiquitin-protease system, which flags proteins for destruction by enzymes called proteasomes. Examples include Arvinas’ PROTACs, Lycia’s LYTACs and C4’s degronimids.
TPDs are a potential fit for “undruggable” diseases like Alzheimer’s because they can selectively degrade proteins that are difficult to target with traditional small molecules, as researchers have pointed out. But, so far, they haven’t been successful.
That’s because other TPDs aren’t targeting the right form of the protein, the Kyung Hee University team claimed in its paper. Many proteins undergo post-translational modification after they’re created; besides being folded, chemicals and complexes may be added to them to make them more stable or activate them.
That’s the case with p38 MAPK, which is thought to trigger pathological processes in Alzheimer’s. After translation, p38 MAPK is activated through a process called phosphorylation, where a phosphate group is added that changes the protein’s shape. This renders drugs targeting the prephosphorylated form of p38 ineffective.
To get around this, the Kyung Hee University researchers ran analyses on a series of p38 MAPK inhibitors they’d developed in an earlier study to see whether any could target the enzyme in its phosphorylated form. One of them, PRZ-18002 was effective, and was also specific enough that it could inhibit p38 MAPK without affecting other enzymes—past p38 MAPK inhibitors caused off-target effects.
Next, the researchers tested PRZ-18002 in brain cells called microglia, which are thought to play a role in the neuroinflammation cascades that, in theory, lead to Alzheimer’s. After finding that the drug selectively reduced phosphorylated p38 in the cells, they moved on to testing it in astrocytes, neuroblasts and hippocampal neurons in mice. PRZ-18002 inhibited phosphorylated p38 in every case and in turn reduced the presence of inflammatory molecules.
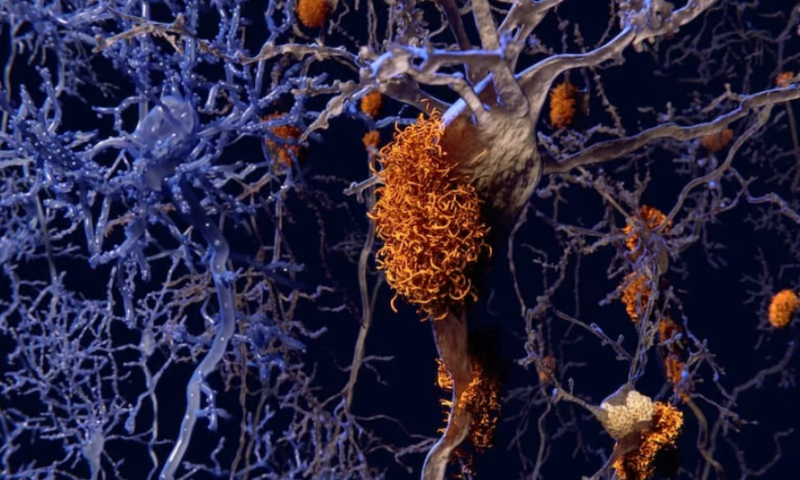
The scientists then moved to testing the compound in mice. They administered PRZ-18002 intranasally to mouse models of Alzheimer’s for one month, then subjected them to the Morris Water Maze test—an experiment used to evaluate spatial learning and memory. The treated mice outperformed untreated models on the test. Subsequent analyses of the mice’s brain tissue showed that the animals that received the drug also had lower levels of amyloid beta plaques in the hippocampus and cortex compared to the untreated group, along with fewer inflammatory molecules in the same regions. The researchers also noted that the treated models had fewer tau tangles, suggesting it might be working via that mechanism, too.
“Collectively, our findings suggest that TPD technology can target a specific [post-translated modification] to induce selective degradation of neurodegenerative disease-associated proteins such as [phosphyorlated] p38, demonstrating its potential as a therapeutic modality against [Alzheimer’s disease],” the researchers concluded in their paper.