The World Health Organization (WHO) has called out Big Pharma for its dearth of antibiotic innovation amid a growing threat of antimicrobial resistance (AMR).
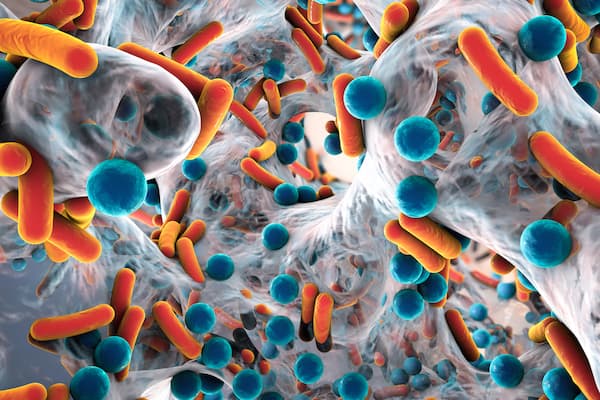
Two new reports out—”Antibacterial Agents in Clinical Development – An Analysis of the Antibacterial Clinical Development Pipeline” and its companion publication, “Antibacterial Agents in Preclinical Development – An Open Access Database”—have highlighted “a weak pipeline for antibiotic agents,” WHO said, with the 60 products in development (50 antibiotics and 10 biologics) bringing “little benefit over existing treatments and very few target the most critical resistant bacteria (Gram-negative bacteria).”
It added that while preclinical candidates “are more innovative,” they are of course many years away from gaining approval.
This echoes concerns from across the globe. Last spring, health experts rounded on pharma companies as having “endless talk and no action” when it comes to antibiotic R&D, as governments around the world continue to sound alarm bells over a potential AMR “apocalypse.”
Speaking at a Wellcome Trust meeting in the U.K. last March, Jim O’Neill, a lord, chair of the Chatham House think tank and the man tasked with heading up a British government global review of AMR back in 2016, accused the bigger players in the industry as “spewing out nonsense” about the problem.
He said they are all talk and no action. “If they produced one-tenth of the commitment in their words, we would be getting somewhere,” he said.
The issue for pharma is that there is little to no ROI for antibiotic R&D, given that one of the key things you’d do with these drugs is not give them out readily.
Cancer and rare drug R&D, while costly, will always see a much greater return, so those have become the mainstays of most Big Pharma companies, with only a handful involved in antibiotic work. Most of the innovation, according the reports, are from small and medium-sized biotechs.
There have been very few new antibiotics approved for use over the past 30 years, and AMR, whereby bacteria evolve to not be killed by older antibiotics, could leave open the possibility that once easily treated infections once again become a deadly scourge should new antibiotics not be made.
O’Neill undertook a review of the AMR landscape and found that the threat could kill an extra 10 million people a year by the middle of the century.
O’Neil, also a former Goldman Sachs chief economist, said the economic barriers could be lifted for pharma by so-called play or pay systems, with a levy on all drug sales being slapped on those that do not have antibiotic development programs.
And those who do play could get a bonus payment of between $1 billion and $1.5 billion for any successful new antibiotic drug, incentivizing them financially.
One of the other more radical ideas being put forward, and one that has been spoken of over the years, is to nationalize antibiotic R&D, although this would remove any competitive element and require large sums of taxpayer money.
O’Neill himself said the solution may be to “just take it away from them and take it over.”
Either way, WHO wants solutions. “It’s important to focus public and private investment on the development of treatments that are effective against the highly resistant bacteria because we are running out of options,” said Hanan Balkhy, WHO assistant director-general for antimicrobial resistance, amid the new reports.
“And we need to ensure that once we have these new treatments, they will be available to all who need them.”