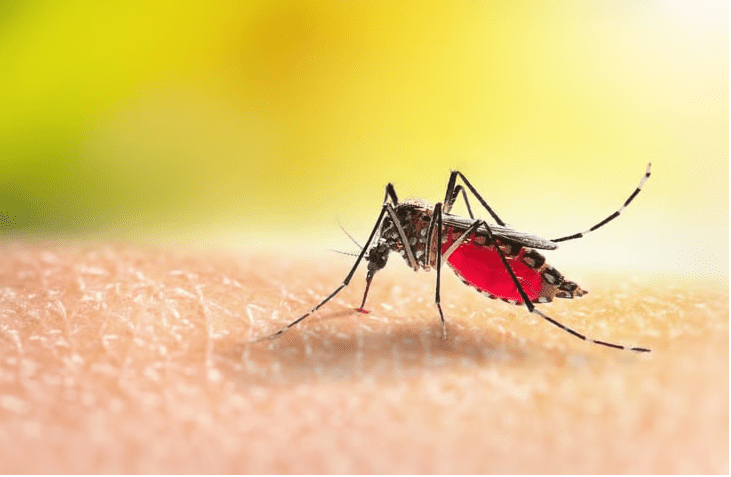
Seven years ago, when the notion of a globe-sweeping coronavirus pandemic was but a remote unease in public health officials’ minds, the Zika virus was inciting panic across South, Central and Latin America. While most who contracted the mosquito-borne pathogen recovered unscathed, the babies of many infected pregnant women were left with serious illness, including severe brain damage.
Now, it appears that an antibody found in pregnant women who were infected with Zika but didn’t pass the virus on to their fetuses can protect mice from the virus and even suppress it to the point that it’s undetectable in their blood. The discovery was described in a study published Nov. 18 in Cell by a research team led by scientists from Weill Cornell Medicine, NewYork-Presbyterian and the National Institutes of Health.
“Vital tools for the next Zika pandemic will be a therapeutic to rapdily clear Zika virus from the blood and a preventative vaccine, both of which can be safely administered to pregnant people,” Sallie Permar, M.D., Ph.D., co-senior author and chair of pediatrics at Weill Cornell, told Fierce Biotech Research in an email.
The study began during the 2015 Zika outbreak in Brazil, where some members of the team were treating patients. They took blood samples to better understand how the patients’ immune systems were responding to the virus, with particular interest in infected pregnant women who did not pass it on to their fetuses. When they analyzed their blood, they found that all of them had something in common: a potent antibody called DH1017.IgM.
The finding was unexpected. DH1017.IgM is an immunoglobulin M, or IgM, antibody. IgM antibodies are released by immune cells called B cells as soon as an infection is detected and are generally weaker than the antibody that comes later (immunoglobulin G, or IgG, antibodies). But in this case, the IgM antibody outperformed its IgG counterpart.
Analyzing the structure of DH1017.IgM revealed a probable explanation. Unlike the IgG antibody, it had multiple “arms” that bent and attached to virus particles simultaneously. This appeared to make it especially potent at neutralizing the virus in cell cultures.
But would it hold up in live animals? To find out, the scientists injected a group of mice with the antibody one day before and one day after infecting them with the Zika virus. While half of the control group died by Day 8—and all of them by Day 10—all the treated mice survived until the end of the two-week observation period. Blood tests showed that the virus particles were undetectable in the experimental group.
The researchers believe the antibody could be used both as a therapeutic agent and a prophylactic given to patients who are at risk of contracting the virus during an outbreak, Permar explained. Next, her team will find out whether it prevents virus transmission from pregnant mice to their offspring. They hope to eventually translate it to the clinic, with an emphasis on ensuring that pregnant individuals are part of the trials—a group that is typically excluded on account of concerns about whether a drug could harm a developing fetus.
“The most devastating effect of Zika infection is the congenital infections, and therefore interventions that are developed must be tested in pregnant people,” Permar said. “While early safety studies should be pursued in non-pregnant people and early efficacy studies should be pursued in pregnant animal models, those interventions that remain promising should move quickly into pregnant women.”
The scientists will also need to persuade potential sponsors that Zika treatments are still worth investigating. Back in 2016, concerns about Zika spreading beyond South, Central and Latin America prompted a flurry of dealmaking for a vaccine between the U.S. government and major names in the pharmaceutical industry, including Sanofi, GSK and Takeda. But as the virus petered out, so did interest in finding a way to prevent it, as The New York Times reported in its investigation earlier this year on children born with the Zika virus. Takeda appears to be the only company still in the running and is currently recruiting for a phase 2 clinical trial on its inactivated virus vaccine (the same strategy used in the hepatitis A, flu injection and rabies vaccines).
More preclinical research is underway as well. In January 2022, a team from Texas Biomedical Research Institute and Walter Reed Army Institute of Research reported that it had developed a vaccine that protected mouse fetuses from developing birth defects due to the virus about 80% of the time. Like Takeda’s candidate, that vaccine also uses inactivated Zika virus.