Manipulating the immune system’s T cells so they’re better able to recognize and kill cancer is the backbone of many immuno-oncology developments in recent years, but the treatments are far from perfect and they don’t work in every patient. In an effort to understand why, scientists at Brigham and Women’s Hospital and the Massachusetts Institute of Technology used high-power microscopy to watch breast cancer cells and T cells interact—and they made a discovery that could enhance immuno-oncology treatments.
The team discovered T cells and cancer cells connect to each other with tiny tendrils and that the cancer cells use those connections to suck energy from T cells. They published their observations in Nature Nanotechnology.
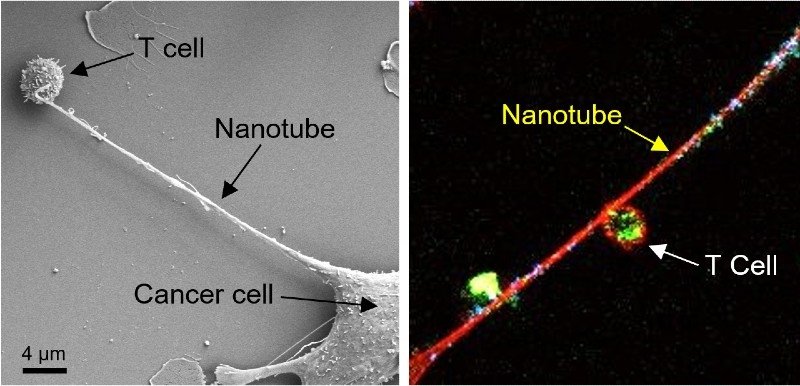
The researchers made the discovery by staining mitochondria—cells’ energy source—in T cells. They discovered that some of the tendrils connecting cancer cells and T cells joined up to form “nanotubes,” they explained in a statement. With the help of a technology called field-emission scanning electron microscopy, they watched as the cancer cells slurped the mitochondria out of the T cells.
The Brigham and Women’s and MIT team wanted to see whether they could prevent cancer cells from hijacking T cells’ energy source. So, they injected a drug into mouse models of lung and breast cancers that inhibited the growth of the nanotubes. Tumor growth slowed, they reported.
Cancer cells rely on mitochondria to fuel their growth and spread, which is why targeting these cellular power plants is a popular idea among oncology researchers. Last year, Swedish researchers reported that drugs they designed to inhibit mitochondrial DNA slowed tumor growth in mice without affecting healthy cells.
In 2019, IBM worked with researchers at Mount Sinai to demonstrate that variabilities in the quantity of mitochondria in cancer cells affected how they reacted to drug treatments.
The Brigham and Women’s and MIT researchers hope their study will inspire new ideas for immuno-oncology combination treatments. “Based on our observations, there is evidence that an inhibitor of nanotube formation could be combined with cancer immunotherapies and tested to see if it can improve outcomes for patients,” said lead author Tanmoy Saha, Ph.D., a postdoctoral researcher at Brigham’s Center for Engineered Therapeutics.